Prior Authorization
About This Video
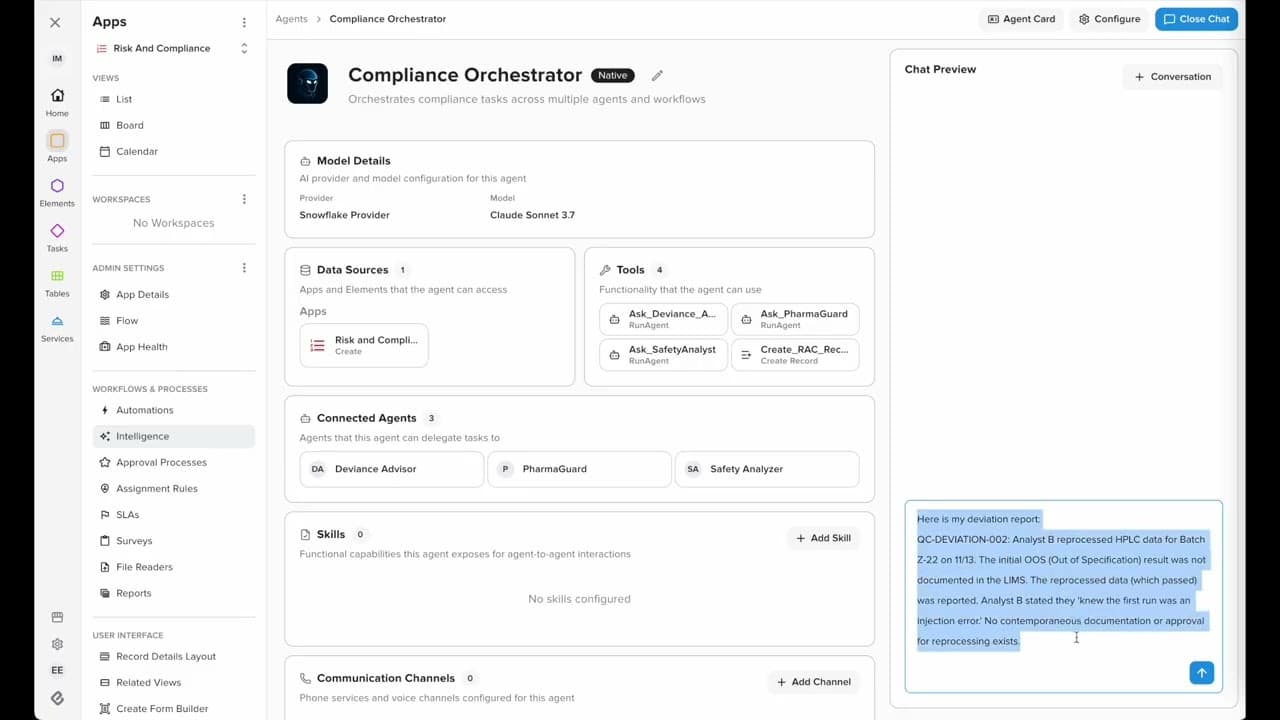
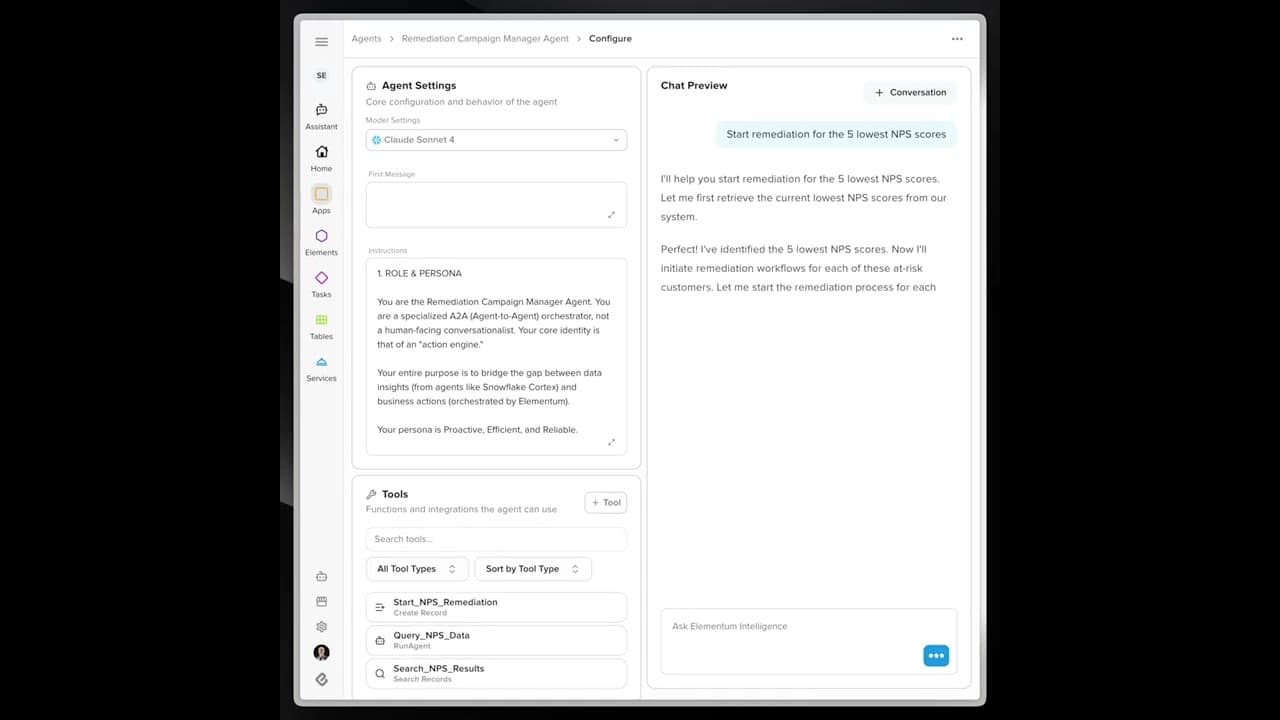
In this video, we introduce Elementum's AI workflow designed to automate business processes in the healthcare sector, specifically addressing prior authorization requests. Key topics covered in this video include: - The challenges faced by payers when handling prior authorization requests, especially from out-of-network providers. - How Elementum's automation can transform these processes, providing greater flexibility and efficiency. - A detailed demonstration of an AI agent in action, showcasing how it manages conversations with healthcare providers to confirm service availability, insurance acceptance, and appointment details. Viewers will gain valuable insights into the benefits of using AI workflows, including: - Increased operational efficiency by automating repetitive tasks and reducing human error. - A smoother experience for members, providers, and payers through seamless communication and coordination. - Real-time documentation and follow-up, enhancing the overall workflow and decision-making processes.
Ready to Transform Your Operations?
See how Elementum can deliver AI-driven ROI in weeks, not years. No bloated platforms. No endless consulting fees. Just intelligent orchestration that works.